Active acne is a common reason patients seek noninvasive treatments. This article examines salicylic acid peels in depth and compares them with microneedling, laser facials, RF, and LED therapy. You’ll learn how each option works, who benefits most, typical downtime, expected results, and safety tips to help decide whether salicylic peels are the best choice for your acne.
Noninvasive skin rejuvenation: Mechanism and Science
Salicylic acid (SA) remains the gold standard in chemical peeling for acne vulgaris because of its unique chemical structure. Unlike alpha-hydroxy acids (AHAs) such as glycolic acid, which are water-soluble, salicylic acid is a beta-hydroxy acid (BHA) and is lipophilic. This means it dissolves in oil.
This lipophilic nature allows the acid to penetrate through the lipid layers between skin cells and travel deep into the pilosebaceous unit (the pore). It does not just exfoliate the surface; it enters the pore itself. Once inside, it performs three distinct actions:
- Comedolytic: It dissolves the intercellular “glue” holding dead cells together to unclog the follicle, effectively treating blackheads and whiteheads.
- Keratolytic: It causes the shedding of the outer layer of skin (stratum corneum), promoting cell turnover.
- Anti-inflammatory: Because salicylic acid is chemically related to acetylsalicylic acid (aspirin), it provides a potent anti-inflammatory effect, reducing the redness and swelling associated with active lesions.
Concentrations and Formulations in Clinical Practice
In a professional setting, we typically utilize SA concentrations between 20% and 30%. This range is considered medium-depth for superficial peeling and is significantly stronger than the 0.5% to 2% found in over-the-counter washes or spot treatments.
The vehicle—the solution the acid is suspended in—matters as much as the percentage. Traditional formulations use an ethanol base. When applied, the alcohol evaporates, leaving the salicylic acid to crystallize on the skin. Newer formulations in 2025 often use supramolecular technology or gel vehicles. These allow for a more controlled release of the acid, reducing the stinging sensation without compromising efficacy.
The pH of the solution is another critical factor. A lower pH (usually around 2.0 to 3.0 for professional peels) increases the free acid value, making the peel more aggressive. Buffered solutions with a higher pH are safer but less effective for severe impaction.
Patient Selection and Candidacy
Not every acne patient is a candidate for a high-strength SA peel. Proper selection prevents complications and ensures results. The ideal candidate presents with:
- Oily skin (Seborrhea): The drying effect of SA helps regulate excess sebum production.
- Comedonal acne: Patients with a high volume of blackheads and whiteheads see the fastest improvement due to the comedolytic action.
- Mild to moderate inflammatory acne: The anti-inflammatory properties help calm papules and pustules.
Patients with dry or sensitive skin may find 30% SA too drying. In these cases, we often start with a lower concentration or choose a different agent.
Contraindications and Safety Precautions
Safety protocols are strict. We do not perform these peels on pregnant or lactating women due to the theoretical risk of systemic absorption (salicylism), although this is rare in limited topical application.
Patients currently taking isotretinoin (Accutane) require careful assessment. While historical guidelines suggested a strict 6-12 month wait, updated 2025 procedural dermatology consensus suggests that superficial peels may be safe sooner, often within 1-3 months post-cessation. However, this requires a case-by-case assessment by a clinician to ensure the skin barrier is not compromised.
We also screen for aspirin allergies. Since salicylic acid is chemically related to aspirin, an allergic reaction is possible.
In-Office Protocol: Step-by-Step
A typical session takes about 15 to 20 minutes.
1. Preparation and Degreasing
The skin is cleansed thoroughly. The clinician then degreases the skin using acetone or rubbing alcohol. This step is uncomfortable but vital. If sebum remains on the skin, it creates a barrier that prevents the acid from penetrating evenly.
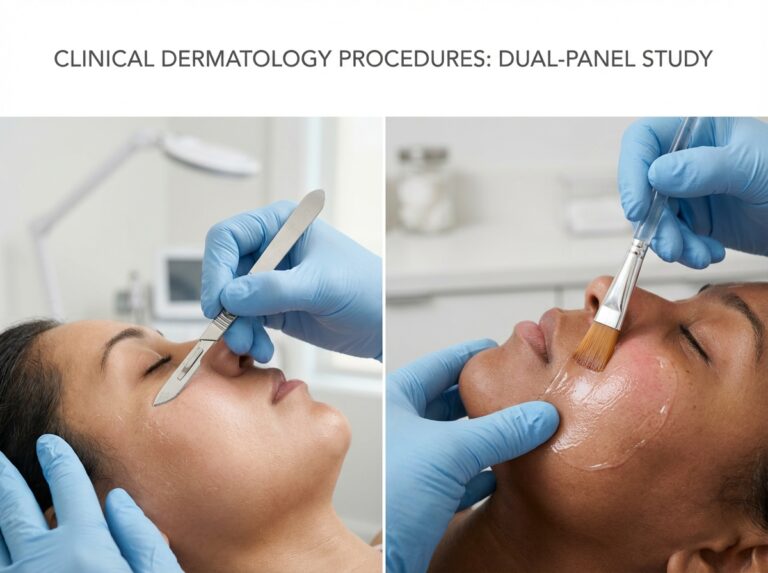
2. Application
The acid is applied with gauze or a brush. Patients experience a sensation of heat and stinging, often described as “ants biting.” This peaks within 2-3 minutes.
3. The “Frost” (Crystallization)
Unlike glycolic acid, salicylic acid is self-neutralizing. As the vehicle evaporates, the acid crystallizes on the surface, forming a white precipitate. This is often mistaken for “frosting” (protein coagulation), but in the case of SA, it is usually just the salt of the acid, known as “pseudofrost.” This confirms even application. True protein coagulation can occur but is less common with superficial SA peels.
4. Neutralization and Cleanup
Since the acid self-neutralizes, we do not need a chemical neutralizer. We simply wash the crystals off with water or a gentle cleanser once the desired time has passed, usually 3 to 5 minutes.
5. Post-Peel Care
We apply a non-comedogenic moisturizer and a mineral-based sunscreen immediately.
Expected Results and Timeline
Results are not instant. Active acne often purges before clearing.
- Week 1: Skin looks dry and may peel. Active lesions might appear more inflamed initially as the pore clears (purging).
- Week 2-3: Reduction in oiliness and drying up of active pustules.
- After 3-4 sessions: Significant reduction in comedones and inflammatory lesions.
A typical series consists of 4 to 6 treatments spaced 2 to 4 weeks apart. Effect of 30% salicylic acid peels in mild to moderate acne vulgaris studies indicate that consistent application yields faster clinical response compared to topical therapy alone.
Downtime and Side Effects
Salicylic acid causes visible peeling. This usually begins 48 hours after the procedure and lasts for 3 to 5 days. The peeling is often flaky rather than sheet-like.
Common side effects include:
- Erythema (Redness): Can last for a few hours to a few days.
- Dryness: Intense skin tightness is normal.
- Post-inflammatory Hyperpigmentation (PIH): This is the biggest risk for darker skin types (Fitzpatrick IV-VI). While SA is safer than glycolic acid for these skin types due to its anti-inflammatory nature, PIH can still occur. We mitigate this by priming the skin with tyrosinase inhibitors (like hydroquinone or azelaic acid) for two weeks prior to the peel.
Comparing SA to Other Modalities
Understanding where SA fits in the treatment hierarchy is essential for setting patient expectations.
SA vs. Glycolic Acid (AHA)
Glycolic acid exfoliates the surface but does not penetrate the pore as effectively. Glycolic is superior for surface texture and anti-aging but inferior for active, clogged pores.
SA vs. Jessner’s Solution
Jessner’s solution contains salicylic acid, lactic acid, and resorcinol. It penetrates deeper and causes more aggressive peeling. Salicylic Acid Peels Versus Jessner’s Solution for Acne Vulgaris data suggests SA is often equally effective for inflammatory acne but with slightly less downtime and irritation than Jessner’s.
SA vs. TCA (Trichloroacetic Acid)
TCA is a protein coagulant. It is excellent for treating acne scarring (ice pick or boxcar scars) but is not the first line of defense for active acne. Using high-strength TCA on active inflamed cysts can cause unpredictable absorption and potential scarring. Efficacy of 25% Trichloroacetic Acid Peel Versus 30% Salicylic Acid trials help delineate these roles, showing SA’s dominance in active lesion reduction.
SA vs. Microneedling and Lasers
We never perform microneedling on active, pustular acne. The needles can rupture the bacteria-filled follicle and spread the infection deeper into the dermis. Salicylic acid is the prerequisite step to clear the active acne. Once the skin is clear of active lesions, we switch to microneedling or fractional lasers to treat the remaining scars.
SA vs. LED Therapy
Blue LED light kills C. acnes bacteria but does not exfoliate or unclog the pore. We often combine these therapies. A patient might receive an SA peel followed by LED light in the same session to target both the hyperkeratosis (clogged pores) and the bacterial load simultaneously.
Summary Comparison Table
| Modality | Best For | Downtime | Risk Profile |
|---|---|---|---|
| Salicylic Acid (20-30%) | Active inflammatory acne, comedones, oily skin | 3-5 days (flaking) | Low; risk of PIH in dark skin |
| Glycolic Acid | Surface exfoliation, mild aging, dullness | 1-3 days (dryness) | Low; requires neutralization |
| Microneedling | Acne scarring, texture (NOT active acne) | 2-4 days (redness) | Moderate; infection risk if active acne present |
| LED (Blue Light) | Adjunct for bacteria reduction | None | Very Low; requires frequent sessions |
Patient Counseling and Management
Patients need to know that their skin will look worse before it looks better. The “purge” is a real physiological response where deep microcomedones surface rapidly.
Key counseling points:
- No picking: Peeling skin must fall off naturally. Pulling it causes scarring.
- Sun protection: The skin is hypersensitive to UV light. Unprotected exposure will lead to dark spots.
- Hydration: The skin will feel tight. Use a basic, fragrance-free moisturizer frequently.
Patient Counseling Scripts
Setting expectations is half the battle. Here is how to explain the process to patients:
- On “Purging”: “You might see your skin get worse before it gets better. This is called purging. The acid speeds up cell turnover, bringing deep clogs to the surface faster than usual. This typically happens after the first peel and clears up by the second or third.”
- On Peeling: “You will likely start peeling around day three. It might look like dry flakes or dandruff on your face. Do not scrub it off. If you pick at the skin while it’s healing, you risk creating a dark spot that takes months to fade. Let the skin shed naturally.”
- On Sun Exposure: “Your fresh skin is defenseless against UV rays. If you go outside without sunscreen in the week following your peel, you are undoing the work and inviting pigmentation. SPF 30 or higher is non-negotiable.”
Photographic documentation is vital. We take photos at baseline and before every subsequent peel. Patients often forget how severe their baseline was once they see improvement, and photos help track the reduction in lesion counts objectively.
Follow-up intervals depend on skin recovery. We do not peel again until the skin has fully recovered from the previous session, which is typically 3 to 4 weeks. Pushing this frequency increases the risk of barrier damage without improving results.
Common questions patients ask about salicylic peels and noninvasive acne care
Patients often arrive at the clinic with a clear goal but a head full of conflicting information found on social media. They want to know if the stinging is bearable or if they can go to work the next day. This section addresses the practical realities of salicylic acid (SA) peels. We strip away the marketing fluff to provide direct answers based on clinical protocols and patient experiences as of late 2025.
Do salicylic acid peels hurt?
Most patients describe the sensation as a sharp stinging or burning feeling rather than deep pain. Unlike glycolic acid which can have a creeping itch, salicylic acid tends to spike in intensity quickly upon application. The discomfort usually peaks within the first two to three minutes. Clinicians often use a handheld fan or cold air device to cool the skin which significantly distracts from the heat.
The sensation subsides rapidly once the peel dries or is neutralized. You might feel a residual warmth or tightness for an hour or two afterward. It feels similar to a moderate sunburn. If you have a low pain threshold, tell your provider. They might adjust the concentration or the number of layers applied during your first visit.
How many sessions are actually needed?
A single peel will exfoliate the skin and provide a temporary glow, but it will not resolve active acne. Acne is a chronic condition that requires consistent management. Clinical data suggests that a series of 4 to 6 treatments spaced 2 to 4 weeks apart is the standard protocol for significant clearance.
Research indicates that 30% salicylic acid peels can be considered as an important adjuvant therapy in mild to moderate acne with visible improvements often noted after the second or third session. Maintenance treatments are usually required every few months to keep pores clear, especially for those with oily skin types.
Are these peels safe during pregnancy?
Salicylic acid is structurally related to aspirin (acetylsalicylic acid). While the absorption from a limited surface area is low, high-concentration peels pose a theoretical risk of systemic toxicity. Most board-certified dermatologists and obstetricians advise against medium-depth salicylic acid peels during pregnancy.
Lower concentrations found in over-the-counter washes (usually 2% or less) are generally considered safe for limited use. For professional chemical peels during pregnancy, clinicians often switch to lactic acid or glycolic acid as safer alternatives. Always clear any cosmetic procedure with your obstetrician first.
Can I get a peel while taking isotretinoin (Accutane)?
For decades the standard rule was to wait six months after stopping isotretinoin before attempting any chemical peel. This was based on fears of scarring and delayed wound healing. Recent procedural guidelines have shifted. Evidence now suggests that superficial chemical peels may be safe for some patients currently on low-dose isotretinoin or those who have recently finished a course.
This is not a decision to make lightly. It requires an experienced provider who can assess your skin barrier function. If your skin is excessively dry or fragile from the medication, a peel will cause injury. Most clinics still prefer a conservative waiting period of 1 to 3 months unless there is a compelling reason to intervene earlier.
Is it safe for darker skin tones?
Salicylic acid is often safer for Fitzpatrick skin types IV through VI compared to glycolic acid. Its anti-inflammatory properties help calm the melanocytes (pigment-producing cells) rather than irritating them. This reduces the risk of post-inflammatory hyperpigmentation (PIH) which is a major concern for patients with darker skin.
Safety depends heavily on the operator. A provider must choose the right concentration and avoid “frosting” the skin too deeply. Pre-treatment with a tyrosinase inhibitor (a cream that stops pigment production) for two weeks prior to the peel is a common strategy to further minimize risk. Always ask your provider about their experience treating your specific skin type.
What is the difference between salon, at-home, and professional peels?
The main differences are pH levels and concentration. Professional peels typically use 20% to 30% salicylic acid with a low pH (around 2.0 to 3.0). This acidity allows the molecule to penetrate deep into the pore to dissolve oil. These require a license to purchase and apply.
At-home “peels” are usually buffered. Even if the bottle says 20%, the pH is often raised to 4.0 or higher to prevent consumer injury. This makes the acid much less active. They work well for maintenance but cannot replicate the results of an in-office procedure. Salon treatments fall somewhere in between, often limited by state regulations on what estheticians can apply versus medical providers.
Can I combine SA peels with retinoids or benzoyl peroxide?
You cannot use them simultaneously. Combining a professional peel with strong home actives is a recipe for a chemical burn. You must stop using topical retinoids (tretinoin, retinol, adapalene) and benzoyl peroxide 3 to 7 days before your appointment. This “rest period” allows your skin barrier to recover so the peel penetrates evenly without causing raw spots.
You can usually resume these products 5 to 7 days after the peel, once all flaking has resolved and skin sensitivity has returned to normal. Your provider will give you a specific timeline based on how your skin reacts.
How long is the downtime?
Salicylic acid is lipophilic, meaning it loves oil. It creates a “frost” on the skin which is actually the crystalized salt of the acid. This looks white immediately after the peel. In terms of social downtime, you will look red and perhaps slightly swollen for 24 hours.
Visible peeling usually starts on day 2 or 3. It typically manifests as flaking around the mouth and nose rather than sheets of skin peeling off. This flaking lasts for 3 to 5 days. Most patients can continue working but may feel self-conscious about the dry texture. Makeup often looks patchy during the shedding phase.
Do insurance plans cover these peels?
In the United States, chemical peels for acne are almost exclusively classified as cosmetic procedures. Insurance plans rarely cover them. You should expect to pay out of pocket. Costs vary by region and provider expertise, typically ranging from $150 to $350 per session. Some clinics offer package deals which can lower the per-treatment cost.
You can use a Health Savings Account (HSA) or Flexible Spending Account (FSA) in some specific cases if a dermatologist deems the peel medically necessary for acne treatment, but this requires a letter of medical necessity and is not guaranteed.
Do SA peels treat cystic acne?
Salicylic acid is excellent for comedonal acne (blackheads and whiteheads) and superficial inflammatory papules. Its ability to penetrate the oil gland helps unclog pores. However, cystic acne occurs deep within the dermis. A surface peel cannot reach the root of a deep cyst.
While SA peels can reduce the surface inflammation associated with cysts, they are rarely a standalone cure for nodulocystic acne. Studies comparing modalities show that 30% salicylic acid peels were effective for inflammatory acne but often need to be combined with oral medications or intralesional steroid injections for deep cysts.
Practical Tips for Pre- and Post-Peel Care
Success relies heavily on how you treat your skin before and after the appointment. Following these steps minimizes complications.
Before the Peel
- Hydrate: Well-hydrated skin heals faster. Drink water and use a basic moisturizer in the days leading up to the treatment.
- Avoid Sun: Do not come in with a fresh sunburn. Providers will turn you away.
- No Waxing: Avoid waxing or threading the face for one week prior.
- Antiviral prophylaxis: If you have a history of cold sores, ask your doctor for antiviral medication to start the day before the peel.
After the Peel
- Gentle Cleansing: Use a soap-free, gentle cleanser and cool water. Do not scrub.
- Moisturize Heavily: Use a bland barrier repair cream. Ingredients like ceramides and hyaluronic acid are safe. Avoid fragrances.
- Sun Protection: Your skin is defenseless. Physical sunscreens (zinc oxide or titanium dioxide) are less irritating than chemical filters immediately post-peel.
- Do Not Pick: This is the most critical rule. Picking at flaking skin can lead to scarring and infection. Let the skin shed naturally.
Red Flags: When to Contact the Clinic
Most side effects are mild, but complications can happen. Contact your provider immediately if you notice specific warning signs. Normal peeling is dry and flaky. If you see yellow or honey-colored crusting, this could indicate a bacterial infection (impetigo). Small, painful fluid-filled blisters may signal a herpes simplex outbreak triggered by the stress on the skin.
Persistent redness that lasts longer than four days or areas that turn dark brown or gray immediately could be signs of a burn or impending hyperpigmentation. Intense itching that keeps you awake is also not normal and may suggest an allergic reaction to a post-peel product. Early intervention prevents long-term damage.
Final takeaways and treatment decision guidance
We have reached the point where information must turn into action. You understand the mechanism of salicylic acid, you know the safety profile, and you have reviewed the common questions regarding pain and downtime. Now the focus shifts to the clinical decision-making process. Choosing the right treatment protocol is rarely about finding a single “magic bullet.” It is about matching the specific pathology of the skin to the correct modality.
Salicylic acid (SA) peels occupy a very specific and highly effective niche in dermatology. They are not the answer for every skin concern, but for the right patient, they offer a balance of efficacy and safety that is hard to beat.
Identifying the Ideal Candidate for Salicylic Acid Peels
The primary strength of salicylic acid lies in its lipophilic nature. Based on clinical data and current practice guidelines in late 2025, the ideal candidate for a professional SA peel presents with:
- Comedonal Acne: Patients with a high density of open comedones (blackheads) and closed comedones (whiteheads). Research indicates that 30% salicylic acid peels were effective for inflammatory acne and more effective than Jessner’s solution peels for treating noninflammatory acne. This makes SA the superior choice for texture issues caused by clogged pores.
- Oily Seborrhea: Individuals with excessive sebum production benefit significantly. The peel creates a drying effect that regulates oil output over time.
- Fitzpatrick Skin Types I-IV: While safe for darker skin with caution, the safety margin is widest in light to medium skin tones.
- Active Papular Acne: Mild to moderate inflammatory lesions respond well because SA is also an anti-inflammatory agent. It helps reduce the redness and swelling associated with active breakouts.
If the primary concern is deep cystic nodules or established pitted scarring, a salicylic acid peel alone will be insufficient. It can be part of a management plan, but it cannot be the monotherapy.
Safety Considerations and Risk Management
Safety is the baseline for any aesthetic procedure. While SA peels are superficial, they are not without risk. The most common adverse event is post-inflammatory hyperpigmentation (PIH), particularly in patients with darker skin tones (Fitzpatrick V and VI).
Key safety protocols include:
- Priming: For patients with melanin-rich skin, clinicians often prescribe a tyrosinase inhibitor (like hydroquinone or non-hydroquinone alternatives) for 2 to 4 weeks prior to the peel to suppress melanocyte activity and reduce PIH risk.
- Isotretinoin Timing: Standard guidelines historically required a 6-month wash-out period after stopping oral isotretinoin before attempting chemical peels. While some newer consensus papers suggest superficial peels might be safe earlier, most conservative practitioners still adhere to a waiting period to avoid delayed wound healing or scarring.
- Pregnancy: Salicylates are generally avoided during pregnancy. While systemic absorption from a small facial peel is low, the theoretical risk leads most providers to recommend lactic or glycolic acid peels instead during gestation.
- Allergies: A true aspirin allergy is a strict contraindication.
When to Choose Alternatives
Knowing when not to peel is just as important as knowing when to peel. There are scenarios where energy-based devices or mechanical treatments offer superior outcomes.
Microneedling
Microneedling is the gold standard for textural repair rather than active inflammation. If the patient has atrophic acne scars (ice pick, boxcar, or rolling scars) but no active pustules, microneedling is the better choice. Performing microneedling over active acne can spread bacteria, whereas SA peels treat the active bacteria.
Laser and Light Therapies
Vascular lasers (like PDL) target the heme in blood vessels. They are superior for treating the persistent redness (post-inflammatory erythema) left behind after acne clears. Furthermore, studies suggest that while acne subjects had significant benefit from the salicylic acid peel alone, they experienced greater significant benefit from PDL treatment combined with the peel.
LED and RF
Blue light LED is a great non-contact adjunct for killing C. acnes bacteria but rarely clears moderate acne on its own. Radiofrequency (RF) microneedling is excellent for deep scarring and tightening but involves higher costs and downtime compared to chemical peels.
Decision Flow for Treatment Selection
To simplify the clinical decision-making process, we can use a tiered approach. This flow helps determine when to start with peels and when to escalate.
Tier 1: Professional SA Peels (The Starting Point)
Patient Profile: Oily skin, blackheads, whiteheads, occasional inflamed bumps.
Action: Series of 4 to 6 peels (20-30% concentration) spaced 2 to 4 weeks apart.
Expectation: Reduction in oil, clearing of pores, faster resolution of active breakouts. Evidence shows that 30% salicylic acid peels can be considered as an important adjuvant therapy in mild to moderate acne with faster clinical response.
Tier 2: Combination Therapy (The Escalation)
Patient Profile: Persistent inflammatory acne, slow response to peels alone, significant redness.
Action: Combine SA peels with LED therapy or IPL.
Evidence: Research indicates that the combination of SSA 30% with IPL compared to SSA 30% alone not only provides better treatment for acne vulgaris but also improves skin barrier function.
Tier 3: Referral or Specialist Care (The Pivot)
Patient Profile: Deep nodules, cysts, immediate scarring upon breakout, or no improvement after 3 months of peels.
Action: This warrants a move to oral medications (antibiotics, hormonal therapy, isotretinoin) or deeper procedural interventions like laser resurfacing.
Practical Next Steps for Patients
If you have decided that a salicylic acid peel is the right next step, preparation ensures the best results. The consultation is your opportunity to align expectations with reality.
Consultation Checklist
Bring this mental or physical list to your appointment:
- Current Topicals: List everything you put on your face. Retinoids (tretinoin, retinol, adapalene) usually need to be stopped 3 to 7 days before a peel.
- Medical History: Disclose any history of cold sores (HSV). A peel can trigger a flare-up, so prophylactic antiviral medication might be prescribed.
- Sun Exposure: If you have a fresh tan or a sunburn, you cannot be treated.
- Patch Test Request: If you have sensitive skin or a history of reactions, ask for a spot test behind the ear or on the jawline before doing the full face.
Recommended Timeframe for Reassessment
Patience is a medical necessity here. Skin cycles take approximately 28 days. You should not judge the success of a peel series after one session.
Commitment: Plan for a 3-month window.
Checkpoint: Evaluate progress after the third peel. If there is zero improvement, the diagnosis or the treatment depth needs to be re-evaluated. However, most patients see a reduction in lesion count and oiliness by this stage.
Shared Decision Making
The era of the doctor dictating treatment without patient input is over. The best outcomes happen when you understand why a treatment is being chosen.
Ask questions. Ask why a 20% peel is chosen over a 30%. Ask why salicylic acid is being recommended over a Jessner’s peel. A qualified provider will welcome these questions because an informed patient is more compliant with aftercare and has more realistic expectations.
Salicylic acid peels remain a cornerstone of acne management in 2025 because they work. They are chemically elegant, targeting the oil and inflammation directly. By understanding where they fit in the hierarchy of treatments—below aggressive lasers but above standard facials—you can make a choice that clears your skin safely and effectively.
References
- Effect of 30% salicylic acid peels in mild to moderate acne vulgaris — Our study showed that 30% salicylic acid peels can be considered as an important adjuvant therapy in mild to moderate acne with faster clinical response.
- Treatment of Acne Vulgaris With Salicylic Acid Chemical Peel … – NIH — Conclusion: While acne subjects had significant benefit from the salicylic acid peel alone, they experienced greater significant benefit from PDL treatment …
- 30% supramolecular salicylic acid peels effectively treats acne … — The global acne-grading system (GAGS) score of patients with acne decreased with 30% SSA treatment. The sebum level in the nose (p < 0.001), …
- Salicylic Acid Peels Versus Jessner's Solution for Acne Vulgaris – Ovid — We found that 30% salicylic acid peels were effective for inflammatory acne and more effective than Jessner's solution peels for treating noninflammatory acne.
- Efficacy of 25% Trichloroacetic Acid Peel Versus 30% Salicylic Acid … — To compare the efficacy of 25% trichloroacetic acid peel versus 30% salicylic acid peel in mild to moderate acne vulgaris.
- Clinical Efficacy of a Salicylic Acid–Containing Gel on Acne … – NIH — Following the follow‐up period, sebum levels decreased by 23.65% (p < 0.05), while skin hydration increased by 40.5% (p < 0.05). TEWL decreased …
- Efficacy of Supramolecular Salicylic Acid 30% Combined with … — The combination of SSA 30% with IPL compared to SSA 30% alone not only provides better treatment for acne vulgaris but also improves skin …
Legal Disclaimers & Brand Notices
The content provided in this article is for informational and educational purposes only and does not constitute professional medical advice, diagnosis, or treatment. Discussing specific medical procedures, including chemical peels, laser therapies, and microneedling, involves inherent risks and recovery protocols that vary by individual. Always seek the advice of a board-certified physician or other qualified health provider with any questions you may have regarding a medical condition or treatment plan. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
All product names, logos, and brands mentioned in this text are the property of their respective owners. All company, product, and service names used in this article are for identification purposes only. Use of these names, logos, and brands does not imply endorsement or affiliation.