Chemical peels remain a cornerstone of non-invasive skin rejuvenation. This article explains how AHA, BHA, and TCA peels work, where they fit among microneedling, lasers, RF, and LED, and what to expect regarding indications, downtime, results, and safety. Read on for practical guidance for different skin types and up-to-date best practices for safe, effective outcomes.
Overview of Non-Invasive Skin Rejuvenation
Non-invasive skin rejuvenation has expanded into a massive ecosystem of devices and topical solutions. Patients often feel overwhelmed by the menu of options at a dermatology clinic or medical spa. You have machines that flash lights, devices that poke holes, and wands that emit heat. Amidst high-tech hardware, chemical peels remain a cornerstone therapy. Understanding where peels fit requires looking at the broader landscape of how we manipulate skin biology without surgery.
The goal of any non-invasive treatment is controlled injury or stimulation. We trigger the body’s healing response to produce new collagen, elastin, and healthier cells. The difference lies in the delivery method and the depth of impact.
Common Modalities in 2025
Microneedling relies on mechanical stimulation. A device with fine needles creates thousands of microscopic channels in the skin. This physical trauma triggers a wound-healing cascade. It is particularly effective for textural issues like acne scarring and large pores. Unlike heat-based devices, microneedling carries a lower risk of post-inflammatory hyperpigmentation, making it a frequent choice for darker skin tones.
Laser Facials split into two main categories. Non-ablative lasers heat the underlying tissue without destroying the surface. They target water or pigment to stimulate collagen or break up spots with minimal downtime. Ablative lasers vaporize the outer layers of skin. They offer dramatic results for deep wrinkles and significant sun damage but require substantial recovery time.
Radiofrequency (RF) uses electrical energy to generate heat within the dermis. The primary goal here is tightening. The heat contracts existing collagen fibers and stimulates the production of new ones. You will often see RF combined with microneedling to deliver heat deep into the tissue for a dual effect on texture and laxity.
LED Phototherapy is non-thermal and non-invasive. It uses specific wavelengths of light to modulate cell activity. Blue light targets acne-causing bacteria. Red light reduces inflammation and stimulates fibroblast activity. It is often an add-on therapy rather than a standalone transformative treatment.
Chemical Peels use acids to dissolve the bonds between skin cells. This is chemical exfoliation rather than thermal or mechanical. Peels are unique because they offer a versatile depth of penetration based on the solution used. They can be superficial for a glow or deep for structural remodeling.
Choosing the Right Tool
Selecting a modality depends on the specific skin concern, the patient’s downtime tolerance, and their Fitzpatrick skin type.
Texture and deep scarring often respond best to the physical remodeling of microneedling or the intensity of ablative lasers. Pigmentation issues are tricky. Lasers target specific chromophores (colors) in the skin, which makes them excellent for distinct sun spots. However, for hormonal pigment like melasma, heat from lasers can sometimes worsen the condition. Chemical peels are often the safer, more effective choice for melasma because they exfoliate pigment without generating heat.
Skin type is the critical safety factor. Fitzpatrick types IV through VI (olive to deep skin tones) have more active melanocytes. Heat-based treatments like certain lasers pose a risk of burning or causing dark spots in these patients. Chemical peels, specifically those formulated for diverse skin types (such as Mandelic acid), and microneedling are generally safer alternatives.
The setting matters too. A medical spa might offer superficial peels and non-ablative lasers. A dermatology office is necessary for deep phenol peels or fully ablative laser resurfacing due to the need for anesthesia and medical monitoring.
Comparison of Modalities
This table outlines general expectations for these treatments. Keep in mind that individual experiences vary based on the intensity of the specific protocol used.
| Modality | Primary Indications | Typical Downtime | Avg. Sessions |
|---|---|---|---|
| Chemical Peels | Acne, melasma, texture, fine lines, radiance | 0 to 21+ days (varies significantly by depth) | 3 to 6 (spaced 2-4 weeks apart) |
| Microneedling | Acne scars, pore size, texture | 24 to 72 hours (redness) | 3 to 6 (spaced 4-6 weeks apart) |
| Non-Ablative Laser | Fine lines, mild pigment, general rejuvenation | 1 to 3 days (mild swelling/redness) | 4 to 6 (spaced 4 weeks apart) |
| Ablative Laser | Deep wrinkles, severe sun damage, scars | 1 to 2 weeks (significant peeling/oozing) | 1 (usually sufficient) |
| Radiofrequency (RF) | Skin laxity, mild tightening | 0 to 2 days (mild redness) | 3 to 6 (spaced 1-2 weeks apart) |
| LED Therapy | Active acne, inflammation, post-procedure healing | None | 6 to 12 (often weekly or bi-weekly) |
Why Peels Remain Essential
With high-tech devices available, some assume chemical peels are outdated. The data suggests otherwise. The US Chemical Peel Market Size & Outlook, 2025-2030 indicates steady growth, driven by the demand for effective, lower-cost non-invasive options. Peels offer benefits that energy devices cannot replicate.
First is the biochemical effect. Salicylic acid, for example, is lipophilic. It dives into the pore to dissolve oil, treating active acne in a way a laser cannot. TCA (Trichloroacetic acid) coagulates skin proteins to force distinct remodeling. This chemical interaction treats the skin condition at a cellular level rather than just heating it.
Second is accessibility. Lasers are expensive to buy and maintain, driving up the cost per treatment. Peels are cost-effective for the provider and the patient. This allows for consistent maintenance treatments, which is often the key to long-term skin health.
Integration and Combination Protocols
Modern aesthetics rarely relies on a single modality. We now see “stacking” or sequential treatments. A common protocol involves using a chemical peel two weeks before a laser or microneedling session. The peel removes the dead stratum corneum. This clears the path for the laser or needles to penetrate more effectively and evenly.
Another approach is alternating months. A patient might do microneedling one month for collagen induction and a chemical peel the next month to maintain surface radiance and pigment control. This targets different layers of the skin over time. Providers also perform “lunchtime” superficial peels immediately before LED therapy to enhance light penetration and calm the skin post-exfoliation.
Chemical peels act as the versatile connective tissue in a skincare plan. They can be the main event or the supporting actor depending on the formulation. Understanding how they function biologically is the next step in mastering their use.
Peel Fundamentals: How Peels Work and Key Terms
Chemical peels rely on a specific biological principle known as controlled injury. While lasers use light and heat to trigger a response, peels use chemical agents to create a wound of a specific depth. The body perceives this injury and initiates a healing cascade. This process stimulates the production of new collagen and elastin while replacing damaged tissue with fresh skin cells.
Understanding the mechanism requires looking at how skin cells hold together. In the epidermis, cells are bound by microscopic structures called desmosomes. Think of these as the glue or velcro keeping the skin barrier intact. Chemical agents work by dissolving this glue or by causing the proteins inside the cells to coagulate. This process is called keratolysis. When the bonds break, the dead outer layers of skin detach and shed. This reveals the newer cells underneath and forces the basal layer of the skin to accelerate cell turnover.
Depth Classifications
We categorize peels by how deeply they penetrate the tissue. This depth determines both the results and the recovery time.
- Superficial Peels: These affect only the epidermis. They target the stratum corneum and sometimes the granular layer. We use these for mild texture issues, minor pigment irregularities, and refreshing the skin glow. The injury is minimal. You might see mild flaking or no visible peeling at all.
- Medium Depth Peels: These penetrate through the epidermis and reach the upper reticular dermis or papillary dermis. This is where the real remodeling happens. The chemical causes protein coagulation in the skin layers. This triggers a stronger inflammatory response which leads to significant collagen stimulation. These are effective for deeper wrinkles, acne scarring, and significant photodamage.
- Deep Peels: These reach the mid-reticular dermis. They historically used phenol or croton oil. They offer dramatic results but carry high risks of scarring and hypopigmentation. In modern practice, deep laser resurfacing has largely replaced deep chemical peels due to better safety profiles, though phenol peels are still performed by specialized surgeons.
The Science of Formulation: pH and Concentration
A common misconception is that the percentage of the acid is the only thing that matters. In reality, the pH level is equally important. The acidity of a solution determines its strength. This relationship is defined by the pKa value of the acid. The pKa is the pH at which half the acid is free to penetrate the skin and half is buffered.
For an acid to be effective, the pH of the formula must be lower than the pKa of the acid. If you have a 20% glycolic acid peel with a pH of 4.0, it will be very mild because most of the acid is neutralized. The same 20% glycolic acid at a pH of 1.5 is extremely potent and could cause a burn if not managed correctly. This is why professional peels differ vastly from over-the-counter versions even if the percentage on the bottle looks the same.
Key Terminology
You will hear specific terms used during a treatment. Knowing them helps manage expectations.
Neutralization refers to stopping the chemical reaction. Some acids like glycolic acid require the application of water or a bicarbonate solution to stop them from penetrating further. Others like salicylic acid or TCA are self-neutralizing. They stop working once they have reacted with the proteins in the skin or the solvent evaporates.
Frosting is a white appearance on the skin that occurs during medium or deep peels. It looks like a thin layer of snow. This is not the product drying on the skin. It is the visible sign of protein coagulation (denaturation) in the epidermal or dermal layers. It indicates the endpoint of the peel has been reached. A solid white frost usually means a deeper injury than a patchy frost.
Epidermal Sloughing is the shedding process that happens days after the treatment. The dead skin turns dark and hardens before cracking and peeling off. It is vital not to pick at this skin to avoid scarring.
Factors Affecting Penetration
The outcome of a peel depends on more than just the liquid in the bottle. The preparation of the skin plays a massive role. The skin has a natural oil barrier called the acid mantle. If an esthetician applies a water-soluble acid like glycolic acid to oily skin without degreasing it first, the acid will not penetrate evenly. Providers use acetone or alcohol to strip these oils before application.
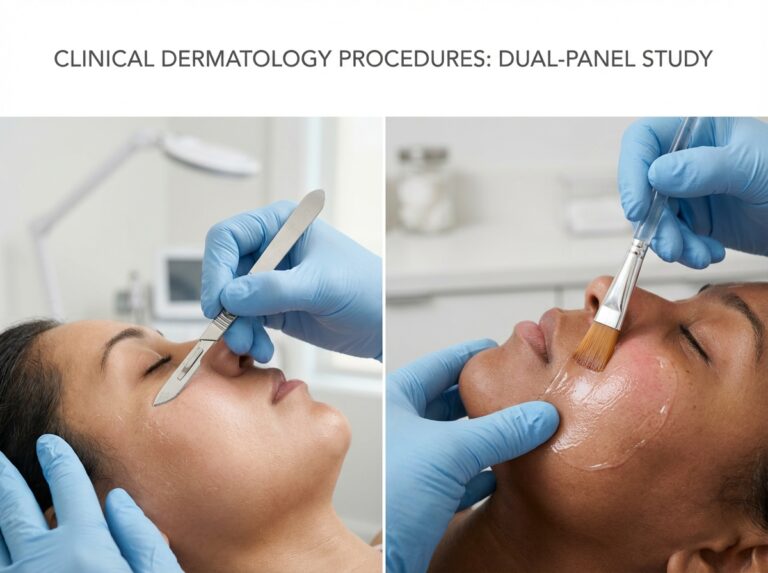
Application method matters too. Applying a peel with rough gauze creates friction and drives the acid deeper than applying it with a soft fan brush. The number of layers applied also increases the depth. A single layer of a modified Jessner’s solution might be superficial, but three or four layers can push it into medium-depth territory.
Provider Types and Regulations
The US Chemical Peel Market Size & Outlook, 2025-2030 indicates a steady rise in demand for these treatments. However, regulations on who can perform them vary significantly by state. Generally, licensed estheticians are permitted to perform superficial peels that affect only the epidermis. They are usually restricted to acids with a pH of 3.0 or higher and concentrations below 30%, though this varies.
Medical professionals such as dermatologists, plastic surgeons, nurse practitioners, and physician assistants can perform medium and deep peels. They have access to unbuffered acids with very low pH levels. In some states, a master esthetician working under the direct supervision of a medical director may perform deeper peels, but the scope is strictly defined by state board regulations.
Over-the-counter products sold for home use are formulated differently. They are buffered to maintain a higher pH. This prevents the acid from penetrating too quickly or too deeply. This safety mechanism ensures that a consumer cannot accidentally give themselves a chemical burn in their bathroom. While these products provide exfoliation, they do not stimulate the deep dermal remodeling seen with professional in-office treatments.
AHA, BHA, and TCA: Specifics and Mechanisms
Alpha Hydroxy Acids represent the most widely utilized category of chemical peeling agents in clinical settings. These water-soluble acids function primarily by diminishing the cohesion of corneocytes at the lower levels of the stratum corneum. They interfere with the ionic bonding of desmosomes which are the protein bridges holding skin cells together. This process induces exfoliation and stimulates the epidermis to accelerate cell turnover. The efficacy of any AHA peel depends heavily on the concentration and the pH of the solution. The free acid value determines the strength. A solution with a pH lower than the pKa of the acid will deliver more free acid into the skin.
Glycolic Acid
Glycolic acid is derived from sugar cane and possesses the smallest molecular weight of all alpha hydroxy acids. This small size allows it to penetrate the epidermis rapidly and deeply. It creates a more intense reaction than other AHAs. Clinicians use glycolic acid to treat photoaging, fine lines, and uneven texture. It also proves effective for comedonal acne by clearing the upper follicular opening.
Typical in-office concentrations range from 20% to 70%. The pH levels for professional glycolic peels usually fall between 0.6 and 2.5. Due to its rapid penetration, glycolic acid requires careful monitoring to prevent epidermolysis or blistering. It must be neutralized with water or a bicarbonate solution to stop the chemical reaction once the desired endpoint is reached. This agent is excellent for exfoliation but requires caution on sensitive skin types.
Lactic Acid
Lactic acid is derived from milk and has a larger molecular structure than glycolic acid. This larger size results in slower and more uniform penetration. It causes less irritation and is often the preferred AHA for patients with sensitive or dry skin. Lactic acid acts as a humectant. It pulls moisture into the skin while exfoliating. This unique property makes it ideal for treating dullness and mild photodamage in patients who cannot tolerate aggressive resurfacing.
Concentrations for professional use typically sit between 30% and 50%. The pH is generally adjusted to be slightly higher than glycolic preparations to maintain a milder profile. It is frequently used to brighten the complexion and improve hydration levels without significant downtime.
Mandelic Acid
Mandelic acid is an aromatic alpha hydroxy acid derived from bitter almonds. It has the largest molecular weight among the common AHAs. The large molecule penetrates the skin very slowly. This slow absorption profile makes mandelic acid an excellent choice for darker skin types (Fitzpatrick IV-VI) as it minimizes the risk of post-inflammatory hyperpigmentation. Mandelic acid also exhibits lipophilic properties unlike other AHAs. It can penetrate the oil in sebaceous follicles to some degree.
This agent is indicated for acne, post-inflammatory hyperpigmentation, and melasma. It has natural antibacterial properties that benefit acne-prone patients. Concentrations usually range from 30% to 50%. It is often left on the skin for a longer duration than glycolic acid because irritation develops much more slowly.
Beta Hydroxy Acids (Salicylic Acid)
Salicylic acid is the primary beta hydroxy acid used in dermatology. Its defining characteristic is lipophilicity. It is oil-soluble. This allows the acid to penetrate through the sebum and deep into the pilosebaceous unit. It is the gold standard for treating oily skin, active acne, and blackheads. Salicylic acid also possesses anti-inflammatory and anesthetic effects. Patients often report a stinging sensation that subsides quickly as the anesthetic property takes effect.
The mechanism of action involves keratolysis and the dissolution of intercellular cement. Professional concentrations typically range from 10% to 30%. The pH of these solutions is usually around 2.0 to 3.0. Unlike glycolic acid, salicylic acid is generally self-neutralizing. The crystallization of the acid on the skin surface signals the end of the reaction. This white residue is often confused with frosting but is actually a precipitate of the salicylic salts. It can be wiped off after the solvent evaporates.
Recent market analysis indicates a sustained demand for acne-specific treatments. The US Chemical Peel Market Size & Outlook, 2025-2030 suggests that specialized formulations for acne management continue to drive segment growth. Salicylic acid remains a cornerstone of these protocols.
Trichloroacetic Acid (TCA)
Trichloroacetic acid is a versatile agent used for superficial to medium-depth peeling. It works by coagulating epidermal and dermal proteins. This process causes the denaturation of proteins which leads to cell death and subsequent regeneration. TCA is not neutralized. The reaction stops when the acid has coagulated the proteins at the depth corresponding to the amount and concentration applied.
TCA is indicated for significant photodamage, actinic keratoses, pigmentary disorders, and textural scarring. It is suitable for most skin types when used at lower concentrations but requires extreme caution in darker skin tones at higher strengths due to the risk of hypopigmentation.
Concentrations determine the depth of injury. Superficial TCA peels use 10% to 20% solutions. Medium-depth peels utilize 20% to 35% concentrations. Solutions above 35% are rarely used as standalone liquid peels due to the high risk of scarring and are often replaced by phenol or combination peels for deeper resurfacing.
Understanding Clinical Endpoints and Frosting
The visual endpoint of a peel guides the clinician on when to stop the application. For AHAs, the endpoint is usually erythema (redness) or a specific time limit. For TCA, the endpoint is frosting. Frosting is the whitening of the skin that occurs when the acid coagulates the proteins.
Level I frosting appears as a faint white haze with erythema showing through. This indicates superficial epidermal peeling. Level II frosting is a solid white coat with no background redness. This indicates the peel has reached the papillary dermis. Level III frosting is a solid enamel-white appearance. This signifies penetration into the reticular dermis and carries a higher risk of scarring. True frosting with TCA must be distinguished from the pseudo-frosting seen with salicylic acid. The latter is simply dried crystals sitting on top of the skin.
Protocols regarding layers and pressure are critical. Applying multiple layers of TCA drives the acid deeper. Friction or pressure during application also increases penetration. Exact concentrations and application techniques must be determined by trained clinicians based on the individual patient’s skin thickness and history. Up-to-date clinical sources and manufacturer guidelines should always be consulted for precise protocols.
Indications, Expected Results, and Downtime
Knowing what specific skin issues respond best to chemical peeling helps manage expectations before you book an appointment. We often see patients hoping for a facelift effect from a bottle. That is not how this works. Peels rely on exfoliation and regeneration. They improve the quality of the skin envelope rather than changing the structure underneath.
Primary Indications and Realistic Outcomes
You need to match the depth of the peel to the severity of the problem. A light enzyme peel will not remove a deep boxcar acne scar.
Acne and Acne Scarring
Active acne responds well to salicylic acid peels. The acid cuts through oil and reduces inflammation. You typically see a reduction in active breakouts within a few days of the first session. It dries out pustules and unclogs pores.
Timeline and Sessions:
Most people need a series of 4 to 6 treatments spaced 2 to 4 weeks apart.
Realistic Outcome:
Expect clearer skin and fewer future breakouts. Deep pitted scars require medium-depth TCA peels or combination therapy. A single superficial peel will not erase pitted scarring.
Fine Lines and Surface Texture
Rough skin texture and very fine static lines improve with glycolic or lactic acid. These acids dissolve the glue holding dead cells together. The skin reflects light better after these cells shed.
Timeline and Sessions:
Maintenance is key here. A series of 3 to 6 peels is standard.
Realistic Outcome:
Skin feels softer and looks brighter immediately after healing. Deeper wrinkles or dynamic lines from muscle movement will not disappear.
Uneven Pigmentation and Melasma
This is the most difficult condition to treat. Melasma is heat-sensitive and hormonal. Aggressive high-heat lasers can sometimes make it worse. Chemical peels offer a non-thermal alternative. Mandelic acid and modified Jessner’s solutions are common choices.
Timeline and Sessions:
Treatment is slow. You might need 6 or more sessions spaced 4 weeks apart.
Realistic Outcome:
Pigment lightens gradually. You must use strict sun protection or the pigment will return instantly. Complete permanent removal of melasma is rarely promised. Management is the goal.
Sun Damage and Pre-Resurfacing
Widespread sun damage manifests as leathery texture and solar lentigines. Medium-depth TCA peels are the gold standard here. Some providers use lighter peels to prep the skin before a laser resurfacing procedure. This clears the surface debris so the laser penetrates more effectively.
Downtime and Recovery Stages
Recovery varies significantly based on the acid strength and pH. The term downtime can mean anything from slight pinkness to full skin shedding.
| Peel Depth | Typical Downtime | Physical Symptoms |
|---|---|---|
| Superficial | 1 to 7 days | You might look slightly sunburned for 24 hours. Flaking is usually mild and powdery. Many people go to work the next day. |
| Medium | 7 to 14 days | Expect significant redness and tightening initially. The skin often turns brown and peels off in sheets starting around day 3 or 4. Social downtime is real. |
| Deep | 14 to 21+ days | Severe swelling and redness occur. Crusting and oozing are possible. Redness can persist for weeks or months. |
Redness or erythema is a sign of inflammation. It is necessary for collagen stimulation but should resolve. In medium peels, the fresh skin underneath will look pink for several weeks. This is normal. If you see purple bruising or purpura, this is less common with standard acids but can happen with phenol or very strong TCA applications.
Variability and Combination Treatments
Your skin type dictates your reaction. Thicker or oily skin often resists peeling more than thin dry skin. Men often have thicker skin and may require a stronger solution to get the same result as a woman.
Combining treatments changes the recovery timeline.
- Microneedling plus Peel: Some providers apply a peel immediately after microneedling. This pushes the acid deeper. It increases the intensity and the peeling. Expect 2 to 3 extra days of downtime compared to microneedling alone.
- Laser before Peel: Doing a laser treatment followed by a peel is aggressive. This is usually reserved for severe photodamage. The downtime is cumulative.
Patient Experience and Pain Management
The sensation during the procedure is often described as “spicy” or stinging.
Superficial Peels:
You will feel prickling or itching. A handheld fan usually makes this tolerable without anesthesia.
Medium Peels:
The burning sensation is more intense. It peaks within a few minutes. Providers might use topical numbing cream beforehand. Some patients take an oral sedative or pain reliever.
Deep Peels:
These require sedation or local nerve blocks. The pain is significant without management.
Blistering and Frosting:
Frosting is a white reaction on the skin. It means the protein in the skin has coagulated. This is a desired endpoint for TCA peels but indicates the peel has penetrated. If you see actual fluid-filled blisters later, contact your provider. That is not a standard peeling reaction and could indicate a burn or infection.
Cost and Value
Prices in the United States fluctuate based on location and provider expertise. The market for these treatments continues to expand as people seek alternatives to surgery. US Chemical Peel Market Size & Outlook, 2025-2030 data suggests a steady increase in demand, which keeps pricing competitive but firm.
Superficial Peels:
Expect to pay between $150 and $300 per session. Since you need a series, the total cost often lands around $1,000.
Medium Depth Peels:
These range from $600 to $1,500 per session. You usually need fewer sessions.
Deep Peels:
These are specialized medical procedures. Costs can exceed $3,000 to $5,000 depending on anesthesia and facility fees.
Chemical peels offer high value for surface-level issues. They are generally cheaper per session than laser treatments. Lasers often start at $600 to $1,000 for even mild resurfacing. For pure exfoliation and brightness, a peel is often the most cost-effective choice. For deep structural tightening, energy-based devices provide better value despite the higher upfront cost.
Safety, Contraindications, and Pre/Post Care
Safety determines the success of a chemical peel just as much as the acid selection. A perfectly executed application can still result in complications if the skin barrier is compromised beforehand or neglected afterward. Understanding who should avoid these treatments and how to manage the recovery phase is essential for preventing long-term damage like scarring or permanent pigment changes.
Contraindications and Risk Factors
Not everyone is a candidate for chemical exfoliation. Certain medical conditions and lifestyle factors significantly increase the risk of adverse events. We categorize these into absolute contraindications, where the treatment must be avoided entirely, and relative contraindications, where caution and physician approval are necessary.
Absolute Contraindications
Active infections act as a hard stop for any resurfacing procedure. This includes bacterial infections like impetigo or viral outbreaks such as Herpes Simplex (cold sores) in the treatment area. Peeling over an active lesion can spread the infection and lead to severe scarring.
Recent use of isotretinoin (Accutane) requires a strict waiting period. This medication suppresses oil gland function and alters wound healing capacity. Most dermatologists mandate a washout period of 6 to 12 months after the final dose before attempting medium or deep peels. Performing a peel too soon carries a high risk of delayed healing and atypical scarring.
Relative Contraindications and Considerations
Pregnancy and breastfeeding require a conservative approach. Salicylic acid (BHA) is structurally similar to aspirin and is generally avoided due to potential systemic absorption. TCA and glycolic acid have better safety profiles but are often postponed until after delivery and lactation to avoid any unnecessary risk or hormonal pigment flares.
Patients with a history of keloids or hypertrophic scarring need careful evaluation. Deep peels are usually unsafe for this group. Uncontrolled diabetes or autoimmune diseases like lupus can impair the immune response and slow tissue regeneration. These conditions do not automatically disqualify a patient but necessitate a modified approach with superficial agents and rigorous monitoring.
Pigmentation Risks in Darker Skin Tones
Post-inflammatory hyperpigmentation (PIH) remains the primary concern for Fitzpatrick skin types IV through VI. The heat and inflammation generated by a chemical peel can stimulate melanocytes to overproduce pigment as a defense mechanism. This results in dark patches that can last months or years.
Reducing this risk starts weeks before the appointment. High-risk patients should precondition their skin using tyrosinase inhibitors. These agents suppress pigment production. Hydroquinone is the gold standard prescription option. Non-prescription alternatives include azelaic acid, kojic acid, or tranexamic acid.
Sun avoidance is critical. Even minimal UV exposure during the healing phase can trigger PIH in sensitized skin. For patients with darker skin tones, we often prefer a series of lower concentration superficial peels rather than a single high-strength treatment. If significant correction is needed for texture or deep scars, alternative modalities like radiofrequency microneedling or specific laser wavelengths often provide a safer safety profile than deep chemical peels.
Pre-Procedure Regimen
Preparation ensures the skin tolerates the acid evenly and heals predictably.
4 Weeks Prior
Start skin preconditioning if you have a history of hyperpigmentation or melasma. This involves applying a melanin inhibitor daily. Daily application of broad-spectrum SPF 30 or higher is mandatory to ensure melanocytes are in a resting state.
7 Days Prior
Discontinue all topical irritants. This includes prescription retinoids (tretinoin, adapalene), high-strength retinol, alpha hydroxy acids, and benzoyl peroxide. Waxing, electrolysis, and depilatory creams must also stop one week before treatment to prevent over-exfoliation.
Patch Testing
A patch test is recommended for new patients or those with sensitive skin. The provider applies a small amount of the peeling agent behind the ear or on the jawline to monitor for excessive erythema or allergic reaction.
Post-Procedure Care Plan
The recovery period requires discipline. The skin barrier is temporarily disrupted. Your goal is to support repair while preventing infection and sun damage.
Cleansing
Wash the face twice daily with cool water and a gentle, non-foaming cleanser. Avoid hot water. Do not use washcloths, scrubbing brushes, or exfoliating sponges. Pat the skin dry with a clean towel. Do not rub.
Moisturizing
Keep the skin hydrated. For superficial peels, a standard fragrance-free moisturizer is sufficient. For medium to deep peels, the skin may feel tight and crack. Use an occlusive ointment or a heavy barrier repair cream to trap moisture and facilitate healing.
Sun Protection
Avoid direct sun exposure completely until the skin has fully re-epithelialized. This usually takes 7 to 14 days depending on the depth. Once the skin heals, apply a broad-spectrum mineral sunscreen with SPF 30 to 50 every morning. Chemical filters can sometimes irritate freshly peeled skin, so zinc oxide or titanium dioxide formulas are preferred.
Managing Peeling and Flaking
Do not pick, pull, or force the skin to peel. Premature removal of dead skin can lead to bleeding, infection, and scarring. If large pieces of skin are hanging and bothersome, you may carefully trim them with sterilized scissors without pulling on the attached skin.
Emergency Signs and Follow-Up
Most side effects are manageable, but specific symptoms require immediate medical attention.
Call your provider if you experience:
- Signs of infection such as yellow discharge, fever, or increasing redness spreading from the treated area.
- Severe pain that is not relieved by over-the-counter pain medication.
- Blistering or crusting that was not discussed as an expected outcome.
- Herpetic breakout (cold sores), which requires immediate antiviral medication to prevent scarring.
Follow-up appointments are typically scheduled one week post-procedure for medium peels to assess healing. Superficial peels may not require a formal follow-up unless complications arise. The United States Chemical Peel Market continues to expand as more patients seek these treatments, making adherence to these safety protocols vital for maintaining high standards of care and patient satisfaction.
Frequently Asked Questions
How do I decide between AHA, BHA, or TCA for my specific skin issues?
You don’t need to guess, but understanding the mechanism helps you have a better conversation with your esthetician. The choice comes down to oil solubility and depth.
Alpha Hydroxy Acids (AHAs) like glycolic and lactic acid are water-soluble. They work on the surface. If your main complaints are dryness, fine lines, or dullness, these are your go-to agents. They exfoliate the top layer to reveal glowy skin without diving deep into the pore.
Beta Hydroxy Acids (BHAs), specifically salicylic acid, are oil-soluble. This is the only option if you have active acne or clogged pores. The acid penetrates through the oil in the follicle to clear out debris. It is also anti-inflammatory, which helps calm red breakouts.
Trichloroacetic Acid (TCA) is a protein denaturant. It doesn’t just exfoliate; it causes controlled injury to force collagen regeneration. This is the heavy lifter for textural issues, deep sun damage, and etched wrinkles. It is stronger and requires more downtime than the others.
Which chemical peel is actually safe for darker skin tones?
This is a critical question because the risk of hyperpigmentation is higher for Fitzpatrick skin types IV through VI. The old myth that dark skin cannot be peeled is false, but the margin for error is smaller.
Mandelic acid is often the safest bet. It has a large molecular structure, meaning it penetrates the skin slowly and evenly, preventing the irritation that triggers pigment response. Salicylic acid is also generally safe because it is self-neutralizing and anti-inflammatory.
You should be very cautious with unbuffered glycolic acid, as it can penetrate unpredictably fast. TCA can be used, but usually at lower percentages (under 15%) or combined with other acids in a blended peel. A provider experienced with melanin-rich skin will often start with a “test spot” near the ear before treating the full face.
How long before a major event should I get a peel?
Never get a peel less than two weeks before a wedding or major photo event. Even a “no downtime” peel can cause unpredictable flaking a few days later. Makeup sits terribly on peeling skin.
For a superficial AHA or BHA peel, schedule it 10 to 14 days prior. This gives your skin time to shed and recover its barrier, leaving you with that fresh glow. If you are doing a medium-depth TCA peel, you need at least four to six weeks. The initial peeling stops after a week, but the underlying redness (erythema) can persist for a month.
Will a chemical peel really get rid of my acne scars?
It depends on the type of scar. If you have post-inflammatory hyperpigmentation (dark spots left behind after a pimple), chemical peels are excellent. They speed up cell turnover and lift that pigment out.
For true textural scars—like icepick or boxcar scars—a standard superficial peel will do almost nothing. You need medium-depth peels or a technique called TCA Cross. In TCA Cross, a high concentration of acid (often 70-100%) is applied precisely into the depression of the scar with a toothpick to stimulate collagen floor-up. This is a medical procedure, not a spa facial.
How many treatments will I need to see a difference?
One treatment is rarely enough unless you are doing a deep, aggressive peel that requires sedation. For standard clinic peels, think in series.
- Acne: Usually a series of 4 to 6 peels spaced 2 to 4 weeks apart.
- Pigmentation: 3 to 6 treatments combined with home care (tyrosinase inhibitors).
- Anti-aging: Maintenance peels every 6 to 8 weeks are common.
Consistency beats intensity. A series of lower-strength peels often yields better, safer results than one aggressive burn.
What are the real risks of scarring or PIH?
Scarring is rare with superficial peels but becomes a real risk if the peel goes too deep or if the skin becomes infected during healing. The most common cause of scarring is the patient picking at the flaking skin. Never pull a flake; cut it with sterile scissors if it’s bothering you.
Post-Inflammatory Hyperpigmentation (PIH) is the most common complication, especially in darker skin or if you go in the sun too soon. This looks like a brown patch where the peel was. It is usually temporary and treatable with creams, but it can last months. Strict sun avoidance is your best defense against PIH.
Can I combine peels with microneedling, lasers, or injections?
You can, but timing is everything. Combining modalities increases efficacy but also inflammation.
Botox/Fillers: You can generally get Botox immediately before a superficial peel or after the skin has healed. For fillers, it is safer to wait until the injection sites have closed and settled (about 1-2 weeks) to avoid infection or moving the product.
Microneedling: Some providers alternate them: Microneedling one month, peel the next. Doing them in the same session is possible but aggressive and increases the risk of PIH. Only advanced providers should stack these.
Lasers: Usually, you do not mix ablative lasers and peels in the same session. Space them out by at least 4 weeks.
I took Isotretinoin (Accutane). How long do I have to wait?
The traditional textbook rule was to wait 6 to 12 months after stopping isotretinoin to avoid scarring. However, recent dermatological consensus suggests this might be overly conservative for superficial peels. Many doctors now perform mild chemical peels 6 months post-treatment.
That said, because isotretinoin alters the oil glands and wound healing capacity, you must disclose this history. Do not try to rush this. If your provider sticks to the 12-month rule, respect that safety margin.
Is it safe to get a peel during pregnancy?
Generally, no. Salicylic acid is structurally related to aspirin and is avoided during pregnancy. TCA and retinoids are also off the table.
Lactic acid is sometimes considered safe by some practitioners because it is naturally occurring in the body, but most clinics have a blanket policy against treating pregnant patients to avoid any liability. Your skin is also more sensitive and prone to melasma (pregnancy mask) due to hormones, so a peel could actually trigger more pigment issues. It is smarter to wait.
What if my skin frosts or stays red for too long?
“Frosting” is a white residue that appears on the skin during the peel. It means different things depending on the acid.
With salicylic acid, the white stuff is often just the salt of the acid crystallizing as the water evaporates. This is harmless. With TCA, frosting indicates protein coagulation—essentially, the acid has reached the intended depth. If you frost immediately or unevenly, the provider will neutralize or stop the application.
If redness persists longer than the expected downtime (e.g., bright red after 2 weeks for a medium peel), this is a red flag for potential scarring or contact dermatitis. Contact your provider immediately. They may prescribe a topical steroid to calm the inflammation.
How do I find a qualified provider?
The US Chemical Peel Market Size & Outlook indicates massive growth, meaning chemical peels are available everywhere from mall kiosks to surgery centers. Availability does not equal safety.
Look for a board-certified dermatologist, plastic surgeon, or a licensed master esthetician working under medical supervision. Ask specifically about their experience with your skin type. If they cannot show you before-and-after photos of someone with your complexion, go elsewhere. Be wary of Groupon deals for deep peels; cheap chemistry on your face is never a bargain.
Final Takeaways and Practical Recommendations
We have covered the science, the chemical differences, and the specific questions you likely had about safety and downtime. You now possess the theoretical knowledge necessary to distinguish a superficial lactic acid refresh from a deep phenol overhaul. Yet information alone does not transform skin. The gap between knowing about chemical peels and actually getting one requires a clear strategy. This final section bridges that gap. It provides a structured approach to making the right decision for your specific skin biology and lifestyle constraints.
The aesthetic market is expanding rapidly. Current data indicates a compound annual growth rate of 4.8% is expected of the United States chemical peel market from 2025 to 2030. This growth means you will encounter more providers and more aggressive marketing. Navigating this landscape demands a focus on safety and realistic goal setting rather than trends.
Selecting the Correct Depth
Your choice of peel depth dictates your results and your recovery. Most dissatisfaction stems from a mismatch here. Patients often expect dramatic results from a superficial peel or underestimate the recovery of a medium one.
Superficial Peels are your maintenance tools. Choose these if you want to brighten skin tone or treat very mild acne. They work on the uppermost layer of the epidermis. You can return to work immediately. The trade-off is that you will need a series of four to six treatments to see significant changes.
Medium Depth Peels address the papillary dermis. This is where collagen stimulation happens. Select this depth for treating sun spots, moderate wrinkles, and acne scarring. You must accept five to seven days of social downtime. The skin will physically shed. This is not a procedure to schedule right before a major event.
Deep Peels are medical procedures. They reach the reticular dermis. These are reserved for severe photoaging and deep scars. They require sedation and weeks of recovery. Do not consider this unless you have exhausted other options and are under the care of a dermatologic surgeon.
Matching Agents to Concerns
The acid you choose acts as the vehicle for your results. While depth matters, the specific chemical agent targets different biological mechanisms.
- Salicylic Acid (BHA) is lipophilic. It loves oil. This makes it the superior choice for active acne and comedones. It dives into the pore to dissolve sebum.
- Glycolic Acid (AHA) has the smallest molecular size of the AHAs. It penetrates fast. This is the standard for general anti-aging and surface texture issues.
- Lactic Acid (AHA) is a larger molecule. It penetrates slower and holds moisture. This is the correct choice for dry or sensitive skin that needs brightening without irritation.
- TCA (Trichloroacetic Acid) is a protein coagulant. It is versatile. At low percentages it glows. At high percentages it restructures collagen. It is the gold standard for texture issues and ice-pick acne scars.
The Safety Protocol
Safety is not just about the procedure. It is about how you manage your skin before and after. Following strict rules prevents post-inflammatory hyperpigmentation and scarring.
Sun protection is absolute. You cannot rely on residual SPF in your makeup. You need a dedicated broad-spectrum sunscreen every single day. UV exposure on peeling skin triggers pigment damage that is difficult to reverse.
Pre-conditioning is often necessary. For medium peels or for darker skin types (Fitzpatrick IV-VI), providers often prescribe a tyrosinase inhibitor like hydroquinone or non-hydroquinone alternatives for weeks prior. This suppresses pigment production and reduces the risk of dark spots.
Do not pick the skin. Premature removal of peeling skin exposes raw tissue. This leads to infection and permanent scarring. Let the skin shed at its own pace.
Your Action Plan
Moving forward requires a systematic approach. Follow these steps to ensure you are prepared.
1. Preparation Phase
Audit your current skincare routine. Stop using retinoids, high-strength acids, and benzoyl peroxide five to seven days before your appointment. Focus heavily on hydration. A compromised moisture barrier increases the risk of adverse reactions.
2. Finding a Provider
Verify credentials. Superficial peels are often safe with licensed aestheticians. Medium and deep peels require medical oversight. Look for a board-certified dermatologist or a plastic surgeon for TCA and phenol treatments. Check their specific experience with your skin type.
3. The Consultation
Ask direct questions. Do not be shy. Ask how many times they have performed this specific peel. Ask to see before and after photos of patients with your skin tone. Ask specifically about their protocol for complications. A good provider knows exactly what to do if the skin frosts too quickly or if a burn occurs.
4. Medical Supervision
Seek a doctor if you have a history of cold sores. You will need prophylactic antiviral medication. Seek a doctor if you have a history of keloid scarring. This changes the risk profile significantly.
Setting Realistic Expectations
Chemical peels are effective tools. They are not magic wands. One treatment rarely fixes a decade of sun damage. Results are cumulative. You build collagen over months. You clear pigment over a series of sessions.
Your skin might look worse before it looks better. Redness, flaking, and temporary darkening of pigment spots are normal parts of the process. Patience is part of the prescription. When matched correctly to your skin type and concern, and when performed with rigorous adherence to safety protocols, chemical peels remain one of the most reliable methods for skin rejuvenation available today.
References
- United States Chemical Peel Market to hit US$2.22 Billion By 2033 — Market Size and Forecast: The Global Chemical Peel Market size reached US$2.45 billion in 2024, up from US$2.22 billion in 2023, …
- US Chemical Peel Market Size & Outlook, 2025-2030 — A compound annual growth rate of 4.8% is expected of the United States chemical peel market from 2025 to 2030. Overview · Dashboard · Statistics · Reports …
- United States Chemical Peel Market Size & Forecast to 2030 — The United States Chemical Peel Market was valued at USD 723.81 Million in 2024, and is expected to reach USD 945.59 Million by 2030, rising at a CAGR of 4.53%.
- Chemical Peel Decade Long Trends, Analysis and Forecast 2025 … — Discover the booming chemical peel market! This in-depth analysis reveals a $337.1 million market in 2025, projected for strong growth …
- Chemical Peel Market | Global Market Analysis Report – 2035 — With a share of 88.2% in North America's chemical peel market generated in 2025, the United States currently dominates the region. It is …
- Chemical Peeling Market Size & Share 2025-2032 – 360iResearch — The Chemical Peeling Market size was estimated at USD 1.28 billion in 2024 and expected to reach USD 1.46 billion in 2025 …
- Chemical peel global market 2016-2026 – Statista — This statistic depicts the worldwide chemical peel facial rejuvenation market from 2016 to 2026. According to the data, the market is expected to grow from.
- United States Chemical Peel Market to Grow with a CAGR of 4.53 … — United States Chemical Peel Market to Grow with a CAGR of 4.53% through 2030 · Relevant Reports · Relevant News.